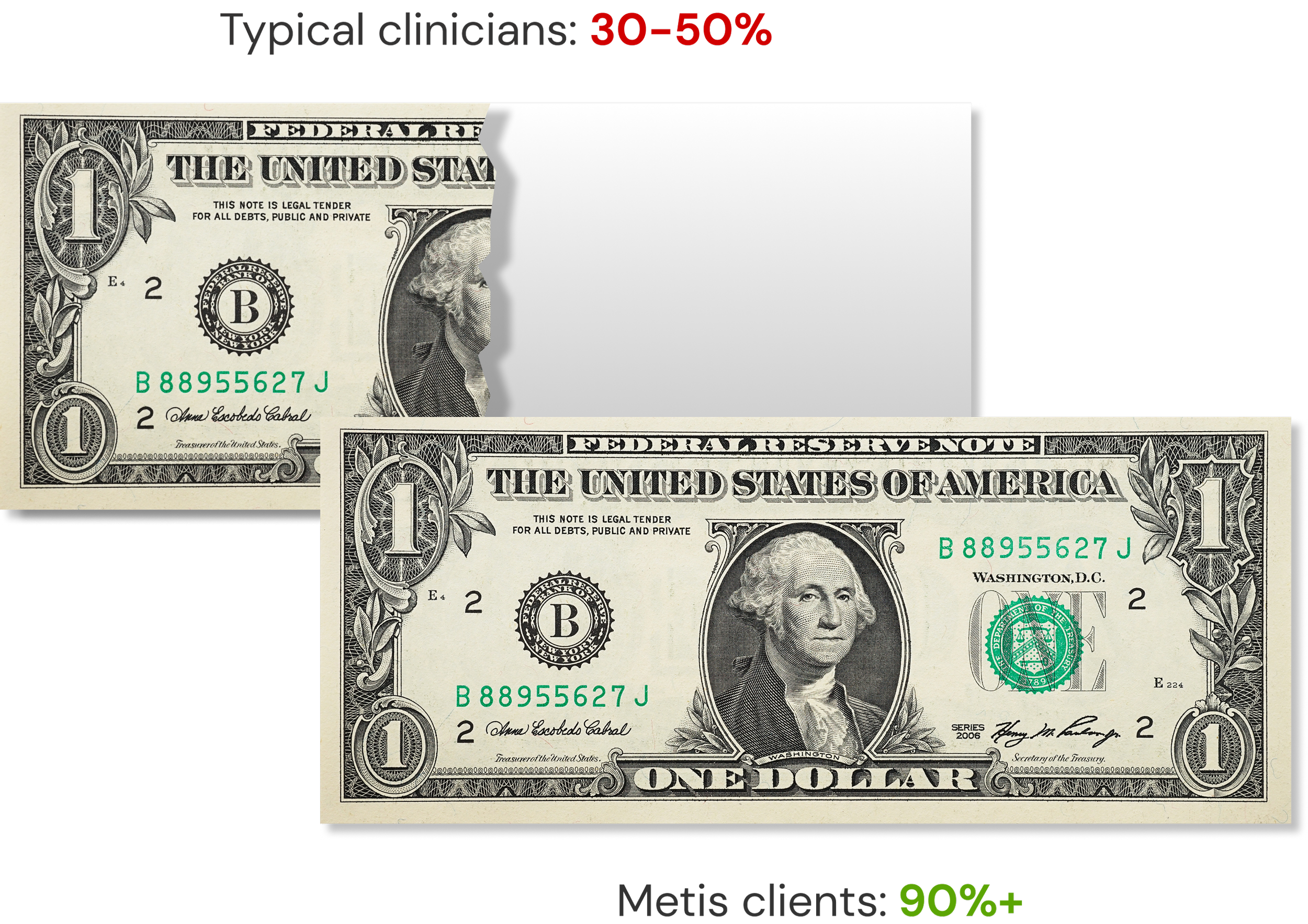
Stop leaving earned revenue on the table
Many clinicians are only collecting 30–50% of what they're owed in parts of their practice, and that’s not okay.
Trusted by healthcare leaders
We support those who care
Scaling is hard enough without payment roadblocks
Whether you’re building a digital platform, delivering virtual care, or using data to drive outcomes, traditional payment systems weren’t built for your model. Credentialing confusion, reimbursement uncertainty, and billing complexity stall growth. Virtual visits face inconsistent payer rules, while data-driven companies struggle with integration and proving ROI. Metis helps by streamlining credentialing, clarifying reimbursement, and simplifying billing workflows. The result is faster payments, predictable revenue, and a longer runway to grow with confidence.
Let's Talk
You care for patients. You deserve to be paid.
Independent clinics operate with limited staff and tight margins. Metis helps by identifying lost revenue across all payers and simplifying claim submission, denial management, and credentialing. Our software highlights underpayments and delays, while our coaching guides staff through contract optimization and streamlined workflows. The result is faster payments, fewer denials, and greater financial independence.
Let's Talk
Coordinated care deserves coordinated revenue
These organizations juggle multiple practices, payers, and value-based contracts on tight margins. Metis helps by uncovering missed revenue, aligning quality with financial goals, and simplifying reporting. Our software highlights underpayments and leakage, while our coaching supports contract optimization, coding accuracy, and practice alignment. The result is stronger network performance, more predictable shared savings, and greater financial stability.
Let's Talk
Mission-driven care deserves financial strength
FQHCs and community health centers serve vulnerable populations with limited staff and resources. Yet complex payer rules, uncompensated care, and value-based care requirements often threaten sustainability. Metis helps by uncovering missed revenue, streamlining credentialing and billing, and aligning quality with reimbursement goals. The result is faster payments, stronger compliance, and more resources to reinvest in your mission of expanding access.
Let's Talk

Our team has worked with thousands of healthcare organizations
Backed by deep experienceFormer SVP at Aledade helping independent primary care providers, directed the $740M Health IT Regional Extension Center Program (part of HHS) supporting 145,000+ providers.
Kim Lynch | CEO
Former VP of Quality & Data Analytics at Corewell Health ($4B system with 8 hospitals and 250 practices), directing programs that secured record-high earnings of $50M.
Amy Kata | Managing Director

Former Chief Data Scientist for a national healthcare account and consulting firm (~$2B Client Portfolio). Led the data unification effort including over 1 Billion Medicaid Claims records from all 50 states.
Dan Roach, M.D. | Advisor
Not your typical healthcare finance partner
We couple AI driven financial analytics software and expert coaching to offer a unique solution to capture more revenue—so you can focus on delivering the care your patients deserve.
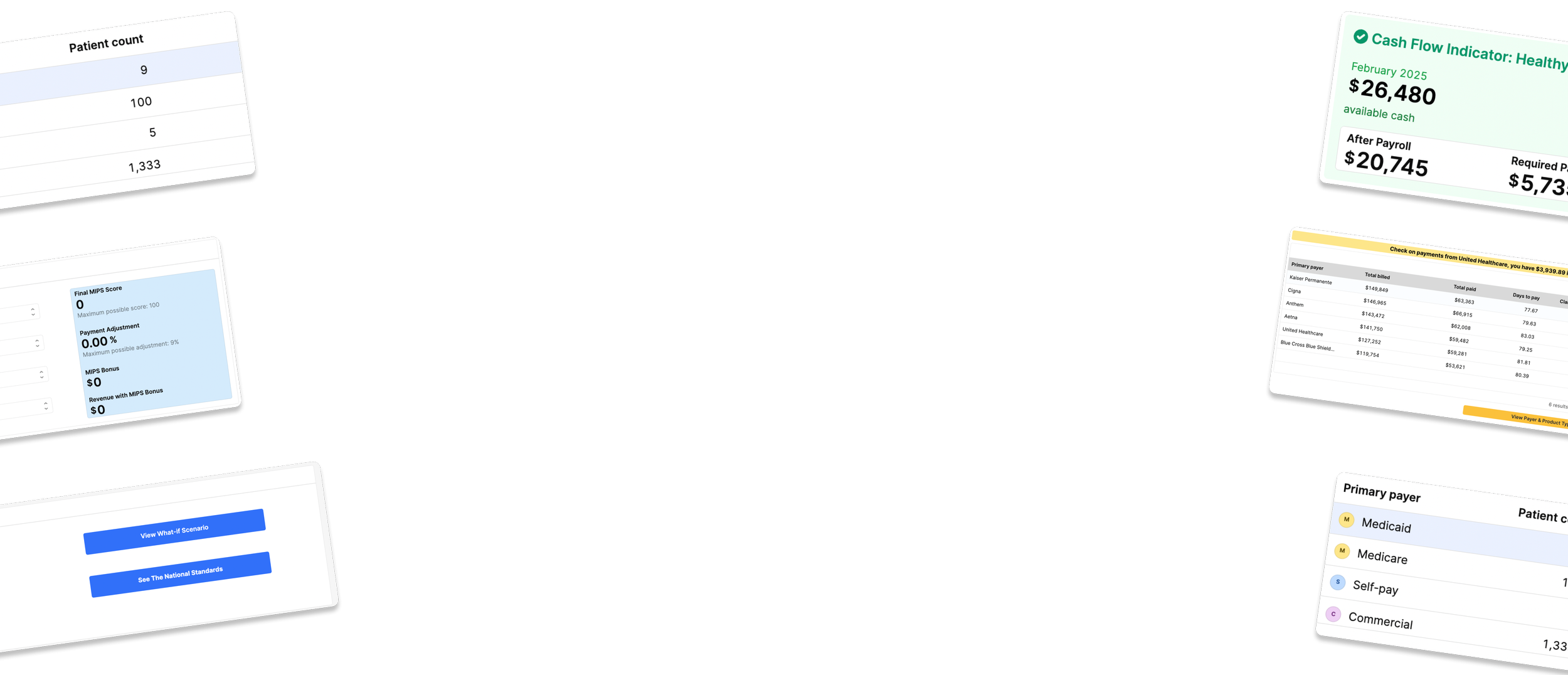
Analytics Software
Explore HiveExpert Coaching
Explore TerraHow much revenue could you gain?
You might be shocked to discover how much money you're already owed but not collecting. Request a free assessment to quantify your opportunity.
Let's Talk- Do you collect less than 90% of what you bill?
- Are you missing quality care metrics?
- Are admin costs increasing as a percentage of revenue?
- Are you staying on top of your credentialing calendar?
- Do your contracts seem fair to your organization?
Expertise that gets you paid
OUR APPROACH
Our methodology systematically identifies and captures revenue you’re already owed but not collecting.

Understand
We show you what’s happening with your money in real time
Align
We help you plan for the future, keeping your team focused and thriving

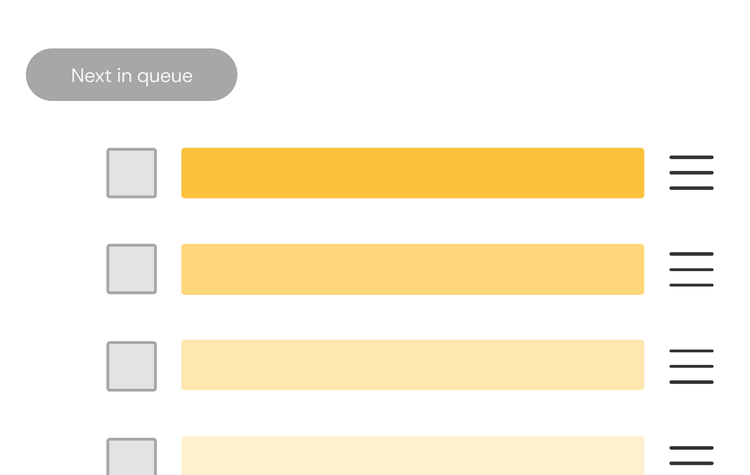
Act
We provide clear next-best-action workflows to help you earn more and work smarter
FAQs
Your questions, answered
We’ve compiled answers to some of the most common questions we hear about our revenue optimization services.
Get In Touch
You deserve to be paid fairly
Healthcare should reward those who deliver care, not those who complicate payment. Our mission is to redirect money from financial intermediaries back to the people actually helping patients. Because every dollar we recover for clinicians is a dollar that can be invested back into patient care instead of subsidizing middleman profits.